People with Parkinson’s benefit from new Home Based Care pathway, UHP supported study shows

The Department of Neurology at University Hospitals Plymouth NHS Trust (UHP) has supported a study which has found that a pioneering care programme through which people with Parkinson’s are supported in managing and monitoring their condition at home has benefits for patients and care teams.
Parkinson’s is the world’s fastest growing neurological condition, with the number of UK patients projected to rise to 170,000 by 2025. However, new research, published in the Journal of Parkinson’s Disease, has assessed the state of health and experiences of people after six months of being cared for under a new Home Based Care programme.
It found that their symptoms were stable, they felt more listened to by – and able to seek help from – health professionals, and reported a far greater sense of autonomy and empowerment than they had under previous treatment programmes.
The quality of care provided to patients was also found to have met 93% of the national audit standards developed by Parkinson’s UK.
Based on the findings, the team who developed the approach say they are now exploring ways in which the NHS can roll the programme out nationally, thanks to funding from NHS England’s Digital Health Partnership Award.
The development of the Home Based Care pathway was initiated by researchers based at the University of Plymouth alongside the Department of Neurology at UHP, with support from The Health Foundation and Parkinson’s UK.
It has also been guided throughout by discussions with people living with Parkinson’s, their families and carers, to ensure it meets their needs and priorities.
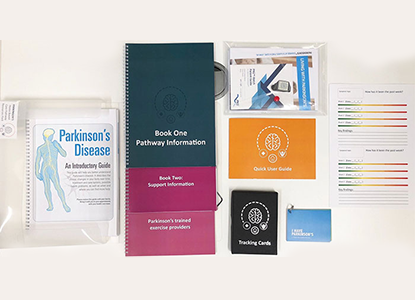
Launched in 2019, the Home Based Care pathway combines at-home monitoring using wrist-worn sensors with support and information on how to recognise and manage different Parkinson’s symptoms, as well as the ability for patients to reach out to healthcare practitioners for support when they need it.
The current study is based on health checks and feedback received from 100 patients being treated by the Parkinson’s service within the Department of Neurology at UHP.
 Camille Carroll, Honorary Consultant Neurologist at UHP, Professor of Clinical Neuroscience at the University of Plymouth and Newcastle University and Joint Clinical Director of the Parkinson’s Excellence Network, is the project lead and senior author on the new study.
Camille Carroll, Honorary Consultant Neurologist at UHP, Professor of Clinical Neuroscience at the University of Plymouth and Newcastle University and Joint Clinical Director of the Parkinson’s Excellence Network, is the project lead and senior author on the new study.
She said: “There is currently a significant unmet need for effective and efficiently delivered care for people living with Parkinson’s. Through this new care pathway, we have shown the benefits of empowering people with knowledge and understanding of their condition. These benefits are felt not only by the people with Parkinson’s and their partners, but also the healthcare teams and organisations providing their care. With support from NHSE Transformation, we are now creating a digital version of this care pathway, which we hope will eventually enable it to be made available through Parkinson’s services across the UK.”
Parkinson’s is the world’s fastest growing neurological condition, with the number of UK patients projected to rise to 170,000 by 2025.
Traditional care comprises regular, in-person clinical reviews by a movement disorders specialist, but current NHS challenges are putting those services under increased pressures.
Dr Rowan Wathes, Associate Director of Policy and Health Strategy at Parkinson’s UK, said: “Parkinson’s UK provides grants to projects that aim to improve Parkinson's health and care services across the UK through the Parkinson’s Excellence Network. We were pleased to award a grant to this project in 2018. The study clearly shows that the remotely-delivered Parkinson's care pathway is a safe and feasible model and we are excited by the potential benefits for people with Parkinson's, particularly those from underserved communities. We look forward to seeing the work progress including the results of formal comparisons with standard care.”
Podcaster and technology writer Rory Cellan-Jones is chairing an Advisory Group looking at ways to roll out the Home Based Care pathway more widely. He said: "People with Parkinson’s know the current model – where you travel to a hospital to see a neurologist once a year, if you’re lucky – is not working for them or their doctors."
"How much better to have a flexible home-based system where you’re able to contact a variety of healthcare professionals as and when the need arises, backed up by new technology to give a far more granular readout of your symptoms than that provided by that annual walk around the doctor’s office. It’s fantastic to see such an approach working for people with Parkinson’s in the south west – the challenge we now need to overcome is how to ensure everyone with the condition, wherever they are living, can benefit in a similar fashion.”
The patient perspective
It is now 13 years since Chris Maycock, who lives with his wife Kay in Cornwall, was diagnosed with Parkinson’s. He experiences tremors in his hands, and many of the other symptoms people might associate with Parkinson’s. But his condition has developed at a different pace – and in different ways – to many other people with Parkinson’s he knows. It is, he says, a clear sign that there is no one-size-fits-all approach to treatment and care.
Ever since his diagnosis, Chris has been a willing participant in research connected to the condition. That has included everything from trials around new drugs to, ultimately, the Home Based Care pathway. He has been part of the HBC pathway for around 18 months, and says it has given him greater confidence in managing his condition.
“I always remember one of my first consultants telling me that I, and my wife, would possibly be the two key people when it comes to managing my Parkinson’s,” Chris says. “So we have always been closely aware of any changes in how I am feeling or behaving, and the HBC programme encourages that as well. It does help you feel more confident and empowered, and I know that if I have any issues the doctors and nurses are just a phone call away.”
Since he was diagnosed, Chris – who spent much of his career working in sales and marketing – has also become involved in a number of patient advocacy groups. These include PenPRIG, through which researchers can discuss projects or results and help members develop a greater understanding of the science behind Parkinson’s.
“Through these groups, people often say to me that they wish the Home Based Care pathway was offered across the UK,” Chris says. “Making more people aware of it, and ensuring they understand what can be gained from it, is always going to be a challenge but hopefully these results will help that.”
Header image credit: University of Plymouth